B116ArevX12
-
Upload
elbuen-john -
Category
Documents
-
view
213 -
download
0
Transcript of B116ArevX12
-
8/11/2019 B116ArevX12
1/20
Como
escribir
y
publicartrabajos
cientficos
J
Fernando
Arevalo
MD
Course
#B116
Sunday,November12
7:308:30AM
Room
#
Hall
G
2006AmericanAcademyofOphthalmology.Allrightsreserved.
-
8/11/2019 B116ArevX12
2/20
Arevalo et al. Trabajos Cientificos/Handout/Pg. 1
Como Escribir y Publicar Trabajos Cientificos
Breakfast with the Experts Roundtable # B116American Academy of Ophthalmology
Las Vegas, NV (November 12th, 2006)
Moderator:
J Fernando Arevalo, MD FACS (Caracas, Venezuela)
-
8/11/2019 B116ArevX12
3/20
-
8/11/2019 B116ArevX12
4/20
Arevalo et al. Trabajos Cientificos/Handout/Pg. 3
7. Cuantos pacientes hacen falta?
8. Que agudeza visual reportar?
9. Cuando hablar de seguro y efectivo?
10.Perseverar!
-
8/11/2019 B116ArevX12
5/20
Journal of Cataract & Refractive Surgery(1.937) was calcu-lated as shown inFigure 1.
For a citation to be included in the calculation, it mustappear in, as well as reference an article published in, 1 ofthe journals in the SCI database. Although citations to allarticles published in the journal are included in the numer-
ator, only specific types of source articles are included inthe denominator. The source articles in the denominator
only include reviews, original research, technical notes,
and case reports. Letters to the editor, abstracts, book re-
views, and editorials are all excluded.12,16
The resulting JIFs greatly vary. The 2004 JCR ScienceEdition displays a positive JIF range from 0.005 to52.431. The list also includes 50 journals with a JIF ozero, or no recorded JIF (JCR 2004, ISI, http://isi1
isiknowledge.com). The latest JIFs (2004) and relatedranking for ophthalmology journals (mean 1.850, range
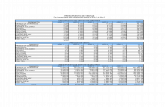
0.081 to 5.345) are illustrated in Table 1. The JIF has
Table 1. The 2004 citation analysis figures including JIF ranking of the 42 journals listed for ophthalmology (SCI-JCR 2004) highlighting total citations for
2004, the JIF, and the immediacy index.
Rank Journal Title Total Cites Impact Factor Immediacy Index
1 Progress in Retinal and Eye Research 1477 5.345 0.826
2 Investigative Ophthalmology & Visual Science 20 456 3.577 0.558
3 Survey of Ophthalmology 2728 3.221 0.163
4 Ophthalmology 15 531 3.210 0.562
5 Archives of Ophthalmology 14 691 2.926 0.311
6 Molecular Vision 935 2.900 0.3017 Experimental Eye Research 5547 2.846 0.374
8 Journal of Refractive Surgery 1830 2.399 0.205
9 American Journal of Ophthalmology 12 937 2.332 0.286
10 British Journal of Ophthalmology 8032 2.000 0.258
11 Journal of Cataract & Refractive Surgery 6021 1.937 0.161
12 Vision Research 12 344 1.812 0.290
13 Journal of Glaucoma 1085 1.730 0.141
14 Visual Neuroscience 2569 1.554 0.264
15 Graefes Archive for Clinical and Experimental Ophthalmology 2933 1.513 0.230
16 Eye 2420 1.496 0.222
17 Optometry and Vision Science 1681 1.360 0.328
18 Cornea 2566 1.290 0.093
19 Ophthalmic Epidemiology 297 1.246 0.03120 Journal of Ocular Pharmacology and Therapeutics 795 1.228 0.069
21 Retina: The Journal of Retinal and Vitreous Diseases 2004 1.207 0.137
22 Current Eye Research 2776 1.097 0.104
23 Clinical and Experimental Ophthalmology 465 1.031 0.362
24 Ophthalmic Research 832 1.000 0.250
25 Acta Ophthalmologica Scandinavica 3000 0.974 0.114
26 Ophthalmic and Physiological Optics 1001 0.925 0.211
27 Journal of Neuro-Ophthalmology 332 0.866 0.227
28 Journal of AAPOS 491 0.761 0.073
29 Japanese Journal of Ophthalmology 919 0.667 0.059
30 Ophthalmic Plastic and Reconstructive Surgery 797 0.667 0.071
31 Ophthalmologica 970 0.645 0.118
32 Ocular Immunology and Inflammation 263 0.562 0.06233 European Journal of Ophthalmology 548 0.534 0.040
34 Ophthalmic Surgery Lasers & Imaging 777 0.508 0.044
35 Journal of Pediatric Ophthalmology & Strabismus 1017 0.490 0.114
36 Klinische Monatsblatter fur Augenheilkunde 1207 0.478 0.098
37 Ophthalmologe 730 0.466 0.069
38 Canadian Journal of OphthalmologyJournal Canadien dOphtalmologie 638 0.442 0.047
39 Journal Francais dOphtalmologie 597 0.267 0.013
40 Neuro-Ophthalmology 172 0.182 0.000
41 Journal of Toxicology. Cutaneous and Ocular Toxicology 65 0.129 0.037
42 Annals of Ophthalmology 704 0.081 0.000
SPECIAL REPORTS: OPHTHALMOLOGY AND VISION SCIENCE RESEARCH
J CATARACT REFRACT SURG - VOL 31, OCTOBER 2005 2001
http://-/?-http://-/?-http://-/?-http://isi1.isiknowledge.com/http://isi1.isiknowledge.com/http://isi1.isiknowledge.com/http://isi1.isiknowledge.com/http://-/?-http://-/?- -
8/11/2019 B116ArevX12
6/20
Full-Thickness Macular Hole after LASIKfor the Correction of Myopia
J. Fernando Arevalo, MD,1 Aristides J. Mendoza, MD,1 Wandsy Velez-Vazquez, MD,2
Francisco J. Rodriguez, MD,3 Alvaro Rodriguez, MD,3 Jose Luis Rosales-Meneses, MD,4 Juan B. Yepez, MD,5
Ernesto Ramirez, MD,6 Amr Dessouki, MD,7 Clement K. Chan, MD,8 Robert A. Mittra, MD,9
Robert C. Ramsay, MD,9 Reinaldo A. Garcia, MD,1 Jos M. Ruiz-Moreno, MD10
Purpose: To describe 19 patients (20 eyes) who developed a macular hole (MH) after undergoing bilateralLASIK for the correction of myopia.
Design: Noncomparative, interventional, retrospective, multicenter case series.Participants: Nineteen patients (20 eyes) who developed an MH after bilateral LASIK for the correction of
myopia at 10 institutions in Venezuela, Colombia, Puerto Rico, Spain, and the United States.Methods: Chart review.Main Outcome Measure: Macular hole development.Results: The MH formed between 1 to 83 months after LASIK (mean, 12.1). In 60% of cases, the MH
developed
6 months after LASIK, and in 30% of cases it developed
1 year after LASIK. Eighteen of 19 (94.7%)patients were female. Mean age was 46 years (range, 2565). All eyes were myopic (range, 0.50 to 19.75diopters [mean, 8.9]). Posterior vitreous detachment was not present before and was documented after LASIKin 55% of eyes. A vitrectomy closed the MH on the 14 eyes that underwent surgical management, with animprovement of final best-corrected visual acuity in 13 of 14 (92.8%) patients. Our 20 eyes with a full-thicknessMH after LASIK reflect an incidence of approximately 0.02% (20/83 938).
Conclusion: An MH may infrequently develop after LASIK for the correction of myopia. Our study shows thatvitreoretinal surgery can be successful in restoring vision for most myopic eyes with an MH after LASIK.
Vitreoretinal interface changes may play a role in MH formation after LASIK for the correction of myopia.Ophthalmology 2005;112:12071212 2005 by the American Academy of Ophthalmology.
Although most macular holes (MHs) are idiopathic and age
related, they also may be associated with myopia, trauma,scleral buckling, pneumatic retinopexy, and vitrectomy.1,2
Tangential foveal traction by the posterior vitreous cortex isregarded as the main cause of full-thickness MHs.3 Re-cently, the prefoveal Mller cell cone has been implicated toplay an important role in this process.4
LASIK has become one of the most popular options for thecorrection of low to moderate myopia worldwide.5,6 However,vitreoretinal complications including endophthalmitis, retinaltearing and detachment (RD), retinal hemorrhaging, and cho-roidal neovascular membrane have been reported.717
Chan and Lawrence18 have reported 3 eyes of 3 myopic
patients who developed an MH in one eye after bilateralLASIK or photorefractive keratectomy. Ruiz-Moreno etal19,20 recently reported a case of an MH in a myopic eyeafter LASIK. We previously reported 10 eyes (10 patients)with full-thickness MH development after bilateral LASIKfor the correction of ammetropia.21
This article reports a larger series of 20 cases of full-thickness MH development after bilateral LASIK for thecorrection of myopia, including 9 from our previously re-ported series and a more detailed description. To our knowl-edge, this is the largest series of this type reported to date.
Originally received: October 13, 2004.
Accepted: January 20, 2005. Manuscript no. 2004-184.1 Retina and Vitreous Service, Clinica Oftalmologica Centro Caracas,Caracas, Venezuela.2 Retina Associates, San Juan, Puerto Rico.3 Fundacion Oftalmologica Nacional, Facultad de Medicina, Universidaddel Rosario, Bogota, Colombia.4 Unidad Oftalmologica y de Cirugia Vitreo-Retina La Colina, San Cris-tobal, Venezuela.5 Clinica de Ojos de Maracaibo, Maracaibo, Venezuela.6 Centro Medico Docente la Trinidad, Caracas, Venezuela.7 Retinal Diagnostic Center, Campbell, California.8 Southern California Desert Retina Consultants, Palm Springs, California.
9
VitreoRetinal Surgery, P.A., Minneapolis, Minnesota.10 Vitreo-retinal Unit, Instituto Oftalmolgico Alicante & Miguel Hernn-dez University School of Medicine, Alicante, Spain.
Presented in part at: American Academy of Ophthalmology Annual Meet-ing, November, 2003; Anaheim, California.
Supported in part by the Fundacion Arevalo-Coutinho para la Investigacionen Oftalmologia, Caracas, Venezuela.
The authors have no proprietary or financial interest in any products ortechniques described in the article.
Correspondence and reprint requests to J. Fernando Arevalo, MD,Clinica Oftalmologica Centro Caracas, Centro Caracas PH-1, Av. Pan-teon, San Bernardino, Caracas 1010, Venezuela. E-mail: [email protected].
1207 2005 by the American Academy of Ophthalmology ISSN 0161-6420/05/$see front matterPublished by Elsevier Inc. doi:10.1016/j.ophtha.2005.01.046
-
8/11/2019 B116ArevX12
7/20
Patients and Methods
Institutional review board/ethics committee approval and patientsinformed consent were obtained for this study. We reviewed themedical records of and obtained follow-up information on allconsecutive patients in our files referred to us with a full-thicknessMH after LASIK between March 1996 and March 2003 at 10institutions in Venezuela, Colombia, Puerto Rico, Spain, and theUnited States. The refractive surgeons who performed LASIK on
the patients who later on developed a full-thickness MH wereasked to provide the total number of LASIK procedures performedduring the study period. A total of 83 938 LASIK procedures(eyes) were performed during the study period (7 years) (Table 1).A preoperative examination, including dilated funduscopy withindirect ophthalmoscopy, and slit-lamp biomicroscopy were per-formed by a retina specialist and/or a refractive surgeon. Patientshad a mean of 41 years of age (range, 1865) and were female in60.7% of cases. Patients underwent surgical correction of myopiaranging from 0.75 to 29.00 diopters (D) (mean, 6.19). Pa-tients were scheduled to be seen during the first postoperative day,at 3 months, at 12 months, and yearly thereafter. Patients wereobserved for a mean of 65 months after LASIK (range, 684).Patients with an MH were included in the study independent of the
length of follow-up.A chart review of cases that developed a full-thickness MHafter LASIK included recording data on gender, laterality, age,preoperative correction (before LASIK), time between LASIK andMH formation (onset of symptoms), fellow-eye status, stage of theMH, presence or absence of yellow deposits on the retinal pigmentepithelium (RPE), presence or absence of epiretinal membrane,diameter of the MH, location of the MH (centric vs. eccentric),presence or absence of subretinal fluid (SRF), presence or absenceof posterior vitreous detachment (PVD) before LASIK and afterLASIK, vitreoretinal procedure performed to close the MH (ifperformed), visual acuity (VA) before and after vitreoretinal sur-gery (if performed), length of follow-up after vitreoretinal surgery(if performed) or MH formation, and type of excimer laser andmicrokeratome used to perform LASIK.
Before LASIK, a retina specialist and/or a refractive surgeonperformed contact or noncontact biomicroscopic evaluation of thefundus to determine posterior vitreous status. After LASIK, aretina specialist performed contact or noncontact biomicroscopicevaluation of the fundus to determine posterior vitreous status andMH characteristics. The presence of a Weiss ring was an importantindex for diagnosing PVD. The data were collected from theclinical record and/or operative report. Optical coherence tomog-raphy was used after LASIK by the retina specialist to confirm theMH and its characteristics.
Selected Case Reports
Case 1A 42-year-old man complained of poor vision in his left eye. Hisocular history included bilateral LASIK for the correction ofmyopia of1.25 D in the right eye and 0.50 D in the left eye onNovember 1998. Eight months after refractive surgery, he pre-sented with a stage 4 MH in the left eye, associated with abest-corrected VA (BCVA) of 20/50. A hyperfluorescent spotcorresponding to the hole was seen on the early frames of thefluorescein angiogram (Fig 1A). During vitrectomy to repair theMH, an optical distortion that originated at the interface of thecorneal cap interfered with intraocular visibility and the surgeonsbinocular depth perception. An iatrogenic retinal tear occurredtemporal to the fovea, and an endolaser was applied. Unfortu-
nately, severe retinal pigment epithelial hyperplasia developed atthe laser site, with mild traction exerted on the fovea ( Fig 1B).Nevertheless, BCVA recovered to 20/25, with MH closure 9months after successful vitrectomy, internal limiting membrane
peeling, and fluidgas exchange.
Case 4
A 30-year-old woman, with 13.00 D of myopia in the right eyeand 10.00 D in the left eye, underwent bilateral LASIK in June2001. Six months after surgery, she noted the onset of blurredvision involving her left eye. Retinal examination revealed a stage4 MH in the left eye (Fig 2A), associated with an RD localized tothe posterior fundus, and a BCVA of counting fingers. An opticalcoherence tomography image showed features of both RD andretinoschisis (Fig 2B). Best-corrected VA recovered to 20/150,with MH closure 4 months after successful vitrectomy and fluidgas exchange.
Case 7
A 57-year-old woman with myopia of16.50 D in the right eyeand 9.00 D in the left eye underwent bilateral LASIK in August2001. Six months after surgery, she noted the onset of blurredvision involving her left eye. Fundus examination revealed a stage4 MH in her left eye, associated with a BCVA of 20/200. Ahyperfluorescent spot corresponding to the MH was seen on thefluorescein angiogram. Optical coherence tomography showed afull-thickness MH with significant surrounding retinal edema andcystic changes. The diameter of the hole measured directly from
Table 1. Cases (Eyes) Contributed by Each ParticipatingCenter
CenterEyes That
Had LASIK*Eyes with
MHs
Clinica Oftalmologica Centro Caracas,Caracas, Venezuela
5720 5
Retina Associates, San Juan, PuertoRico
1221 1
Fundacion Oftalmologica Nacional,Bogota, Colombia
440 1
Unidad de Cirugia Vitreo-Retina LaColina, San Cristobal, Venezuela
240 3
Clinica de Ojos de Maracaibo,Maracaibo, Venezuela
960 1
Centro Medico Docente la Trinidad,Caracas, Venezuela
37 905 1
Retinal Diagnostic Center, Campbell,California
14 400 4
Southern California Desert RetinaConsultants, Palm Springs,California
2880 1
VitreoRetinal Surgery, P.A.,Minneapolis, Minnesota
11 200 2
Vitreo-Retinal Unit, Instituto
Oftalmolgico Alicante, Alicante,Spain
8972 1
Total 83 938 20
MH macular hole.*Total number of LASIK procedures performed during the study period bythe refractive surgeons who performed LASIK on patients who laterdeveloped a full-thickness MH.
Ophthalmology Volume 112, Number 7, July 2005
1208
-
8/11/2019 B116ArevX12
8/20
Figure 1. A, A hyperfluorescent spot (arrow) corresponding to the hole was seen in the early arteriovenous phase of the fluorescein angiogram. B, During
vitrectomy, an optical distortion originating at the interface of the corneal cap interfered with intraocular visibility and the surgeons depth perception.
An iatrogenic retinal tear was created temporal to the fovea, and endolaser was applied. Unfortunately, severe retinal pigment epithelial hyperplasia
developed at the laser site, with mild traction exerted on the fovea. The white reflections superotemporal to the fovea and superonasal to the optic disc
are artifacts.
Figure 2. A, Retinal examination revealed a stage 4 macular hole (arrow) in the left eye associated with a retinal detachment (RD) localized to the
posterior fundus and a best-corrected visual acuity of counting fingers. Posterior staphyloma and myopic chorioretinal and retinal pigment epithelium
(RPE) atrophy are seen. B, An optical coherence tomography image showing features of both RD and retinoschisis. The RPEchoriocapilaris complex
high reflectivity is due to atrophy and choroidal backscatter.
Figure 3. A, Optical coherence tomography (OCT) showed a full-thickness hole with significant surrounding retinal edema and cystic changes. The
diameter of the hole measured directly from the OCT was 390 m. B, Optical coherence tomography after a vitrectomy performed 1 week after
examination closed the macular hole. The fovea regained its normal configuration.
Arevalo et al Full-Thickness Macular Hole after LASIK for the Correction of Myopia
1209
-
8/11/2019 B116ArevX12
9/20
the optical coherence tomography was 390 m (Fig 3A). A vit-rectomy performed 1 week after examination closed the MH (Fig3B), with a BCVA of 20/80 5 months later.
Results
We found 20 eyes (19 patients) with a full-thickness MH afterLASIK (20/83 938), for an incidence of 0.02%. The MH formedbetween 1 to 83 months after LASIK (mean, 12.1). Eighteen(94.7%) patients were female. Mean age was 46 years (range,2565). All eyes were myopic (range, 0.50 to 19.75 D [mean,8.9]). Posterior vitreous detachment was not present before andwas documented after LASIK in 55% of eyes (Table 2). Thevitrectomy closed the MH in all 14 eyes that underwent surgicalmanagement, with an improvement of final BCVA in 13 of 14(92.8%) patients (Table 3).
Table 2 outlines detailed characteristics of MHs in our caseseries. The mean diameter of the MH was 375.4 m, and the rangewas from 100 to 750 m. The MH was centrally located in 19 eyes(95%). The MH was unilateral in 18 of 19 patients (although oneof those patients had an impending MH [stage 1] in the felloweye). A stage 4 MH was found in 12 eyes (60%). There wasabsence of yellow deposits on the RPE of the MH in 17 eyes(85%). Eighteen eyes (90%) lacked a surrounding epiretinal mem-brane. Sixteen eyes (80%) had SRF surrounding the MH; 5 ofthose eyes (all with 10.00D of myopia) had extensive SRF inthe posterior fundus (Table 2).
Discussion
In our study, 20 eyes (19 patients) developed an MH afterbilateral LASIK for the correction of myopia. The MH
formed at a mean of 12.1 months after LASIK. The MHdeveloped within 6 months after LASIK in 60% of cases,and in 30% of cases, the MH developed 1 year afterrefractive surgery. The MHs in our series also developedprimarily in young myopic women with a mean myopia of8.9 D. Typical characteristics of MHs in our series alsoinclude the following: the majority were unilateral, 60%were stage 4, 85% lacked yellow deposits on the base of thehole, and 90% also lacked an associated epiretinal mem-brane. In addition, most were centric holes, with a meandiameter of 375.4 m. Sixteen eyes (80%) had SRF sur-rounding the hole, including 5 eyes (all with 10.00 D ofmyopia) that had extensive SRF in the posterior fundus. Ourfindings support previous studies that showed the charac-teristics and demographics of myopic MHs to differ fromthose of idiopathic MHs. Myopic MHs tend to develop inyoung subjects and may be associated with a rhegmatog-enous RD surrounding the MH.22,23
In the present series, PVD was not present before andwas documented after LASIK in 55% of eyes. Luna et al24
have used kinetic ultrasonography to demonstrate vitreoreti-nal alterations after LASIK, including partial or total PVDin24% (12 eyes) of high myopes. In addition, Kakehashi etal25 have determined that some highly myopic eyes have acomplete PVD with collapse (29.6%) in which the vitreousgel exhibits liquefaction and, therefore, a large retrocorticalspace and smooth movement of the detached vitreous withocular movements. Diffuse chorioretinal atrophy in highmyopia might induce vitreous liquefaction and somehowreduce vitreoretinal adhesion. Their findings are consistentwith similar results in more than half of myopic eyes withMH formation after LASIK in our series. It is possible that
Table 2. Clinical Findings of Patients with Macular Holes (MHs) after LASIK (20 Eyes)
Patient Gender LateralityAge
(yrs)
PreoperativeRefraction
(SE)
Time afterLASIK(mos)
FellowEye
Stageof MH
YellowDeposits ERM
Diameterof MH(m) Location
Cuff ofSRF
PVDbefore
LASIK
PVDafter
LASIK
1 M L 42 () 0.50 8 Stage 1MH
4 No Yes 400 Eccentric No No Yes
2 F L 50 () 3.25 1 2 No No 100 Centric No No No/VMTS
3 F R 32 () 10.00 2 OK 4 No No 100 Eccentric Yes No Yes4 F L 30 () 10.00 6 OK 4 No No 380 Centric PPRD No Yes5 F L 25 () 4.50 1 OK 4 Yes No 400 Centric Yes No Yes6 F R 58 () 10.00 17 OK 4 No No 600 Centric PPRD No Yes7 F L 57 () 9.00 6 OK 4 No No 390 Centric Yes No Yes8 F R 45 () 15.25 30 OK 4 No No 390 Centric Yes No Yes9 F L 34 () 9.00 5 OK 4 No No 500 Centric RRD Yes Yes
10 F R 48 () 8.25 5 Lattice 2 No No 200 Centric Yes No No11 F R 54 () 3.50 6 Lattice 2 No No 200 Centric Yes No No12 F L 35 () 7.75 14 OK 2 No No 200 Centric Yes No No13 F L 52 () 14.50 2 OK 4 No Yes 550 Centric PPRD No Yes14 F L 45 () 7.75 6 15 3 No No 500 Centric Yes No No15 F R 45 () 8.75 11 14 3 No No 400 Centric Yes No No16 F R 51 () 8.00 1 OK 4 No No 400 Centric Yes No Yes17 F R 47 () 15.00 8 OK 4 Yes No 524 Centric No No Yes18 F R 52 () 7.75 18 VMTS 2 No No 200 Centric Yes No No
19 F L 53 (
) 6.75 12 OK 3 Yes No 325 Centric No No Yes20 M R 65 () 19.75 83 OK 4 No No 750 Centric PPRD Yes Yes
ERM epiretinal membrane; F female; L left eye; M male; OK no vitreoretinal pathology/no MH; PPRD posterior pole retinal detachment;PVD posterior vitreous detachment; R right eye; RRD rhegmatogenous retinal detachment; SE spherical equivalent; SRF subretinal fluid;VMTS vitreomacular traction syndrome.
Ophthalmology Volume 112, Number 7, July 2005
1210
-
8/11/2019 B116ArevX12
10/20
in our group of myopic patients with MHs the prevalence ofPVD was enhanced by LASIK surgery, and that PVD mayplay a role in the formation of MHs. However, due to theretrospective nature of our study, the 55% incidence of PVDafter LASIK should be interpreted with caution. Macularhole surgery (MHS) can achieve substantial VA improve-ment for myopic eyes, but the results do not seem to be asfavorable as those reported for typical idiopathic MHs inrecent series.26,27 A vitrectomy closed the MH in all 14 eyesthat underwent surgical management, with an improvementin final BCVA in 13 of 14 (92.8%) patients. However, 6
(42.8%) of 14 eyes that underwent vitreous surgery had aVA of 20/100, and 5 (35.7%) of 14 eyes had a VAoutcome of 20/40. Reasons for poor VA included thedevelopment of cataract and the presence of chorioretinalatrophy. In addition, 4 of our 5 cases of MH and associatedposterior pole RD underwent MHS. All of them ended upwith a VA of 20/150 or worse. Case 18 was our only caseof loss of VA after vitrectomy. However, silicone oil re-moval and cataract extraction are still pending, and couldimprove final VA. Our results should be interpreted withcaution, because multiple surgeons with different surgicaltechniques and training participated in this study. Two of
our patients had to be treated with silicone oil due to theirimpossibility of tolerating prolonged facedown positioning.In addition, internal limiting membrane peeling was per-formed in only 4 of our cases, with trypan blue (Membrane-Blue, DORC International b.v., Zuidland, The Netherlands)or indocyanine green (IC-Green, AKORN Inc., Decatur, IL)staining.
The pathogenesis of MHs (especially idiopathic MHs)remains controversial. Certainly, vitreofoveal traction is feltto be the predominant force, together with preexisting de-
generative changes in the fovea. Chan and Lawrence
18
havestated that LASIK surgery has certain features that mayinduce postoperative vitreoretinal interface changes. Forinstance, the acute intraocular pressure rise associated withthe mechanical stretching of the vitreous base induced bythe suction ring as well as the shock waves generated by theexcimer laser may lead to vitreoretinal traction.10,11,22,23 Inaddition, Ruiz-Moreno et al19,20 recently reported a case ofMH formation in a myopic eye after LASIK. Their reportstated an incidence of 0.01% (1/8972) of an MH afterLASIK. We previously reported 10 eyes with unilateralfull-thickness MH development after bilateral LASIK for
Table 3. Management and Visual Acuity of Patients with Macular Holes (MHs) after LASIK (20 Eyes)
Patient TreatmentVA with before
MH Surgery Final VAFollow-up
(mos) Excimer Laser Microkeratome
1 Vitrectomy gas 20/50 20/25 9 Chiron Technolas Keracor217*
Chiron automated cornealshaper*
2 None 20/50 20/50 1 Ladar Vision 4000 Camazo-Barraquer
3 None 20/200 20/200 2 Nidek EC-5000 Hansatome*4 Vitrectomy gas CF 20/150 4 Nidek EC-5000 Nidek MK-2000
5 Vitrectomy gas 20/200 20/30 7 Nidek EC-5000
Nidek MK-2000
6 None CF CF 17 Nidek EC-5000 Nidek MK-2000
7 Vitrectomy gas 20/200 20/80 4 Chiron Technolas Keracor217*
Chiron automated cornealshaper*
8 None 20/200 20/200 5 Coherent Schwind Keratom II Moria One
9 Vitrectomy gas laser LP 20/200 70 VISX 20/20 Chiron automated cornealshaper*
10 Vitrectomy gas 20/200 20/60 10 Nidek EC-5000 Hansatome*11 Vitrectomy gas 20/200 20/40 6 Nidek EC-5000 Chiron automated corneal
shaper*12 Vitrectomy gas 20/200 20/100 12 Nidek EC-5000 Chiron automated corneal
shaper*13 Vitrectomy gas CF 20/400 28 VISX 20/20 Chiron automated corneal
shaper*14 Vitrectomy ILM gas 20/80 20/40 24 VISX 20/20 Moria One
15 Vitrectomy ILM gas 20/80 20/25 20 VISX 20/20 Moria One
16 None CF CF 12 Nidek EC-5000
Moria One
17 None 5/400 5/400 60 Coherent Schwind Keratom II Moria One
18 Vitrectomy Silicone oil 20/80 20/200 11 Nidek EC-5000 Chiron automated cornealshaper*
19 Vitrectomy ILM gas 20/100 20/50 41 Chiron Technolas Keracor217*
Chiron automated cornealshaper*
20 Vitrectomy ILM Silicone oil
HM 20/200 3 VISX 20/20 Chiron automated cornealshaper*
CF counting fingers; HM hand movements; ILM internal limiting membrane peeling; LP light perception; VA visual acuity.*Baush & Lomb Surgical, Inc., San Dimas, CA.Alcon Laboratories, Inc., Fort Worth, TX.MORIA USA, Doylestown, PA.NIDEK Co., Ltd., Gamagori, Japan.Coherent, Santa Clara, CA.VISX USA, Inc., Santa Clara, CA.
Arevalo et al Full-Thickness Macular Hole after LASIK for the Correction of Myopia
1211
-
8/11/2019 B116ArevX12
11/20
the correction of ammetropia.21 Retinal breaks and RD alsohave been reported to occur after LASIK.1015
An important limitation of our study is that, due to itsretrospective nature, follow-up was not consistent, and it ispossible that patients who developed an MH were seen byother ophthalmologists. Thus, it is possible that the 0.02%rate reported in this study is an underestimation of the trueincidence of MH formation after LASIK. However, in the
participating centers patients with MHs are referred to avery limited group of retina and vitreous specialists, withthe exception of the 3 participating centers in the U.S. Tothe best of our knowledge, no additional cases of MH afterLASIK have occurred in patients from our study group.
Our findings are not generalizable to all myopic eyes thatundergo LASIK. However, myopia is a risk factor for MHformation.2 It is possible that vitreomacular interfacechanges occurring after LASIK may predispose certain my-opic eyes to form an MH. Nevertheless, there are notenough hard data in the literature to determine if these are
just myopic holes that would have developed anyway, re-gardless of LASIK.
In summary, we report 20 eyes of 19 patients with nopresurgical sign of an MH that developed a full-thicknessMH after LASIK. Consistent with previous series, 94.7% ofthe patients developing an MH were women. Our studyshows that vitreoretinal surgery can be successful in restor-ing vision for most myopic eyes with an MH after LASIK.However, final VA may be limited by myopic degeneration,amblyopia, or cataract formation. LASIK should be addedto the list of conditions or surgical procedures that may beassociated with formation of an MH, although its incidenceis very low (0.02%). Our results need to be confirmed byprospective studies to determine a more accurate incidenceof MHs after LASIK. Future prospective investigation in-volving a large number of myopic eyes and with ultrasonicfindings may be valuable for determining vitreoretinal in-terface changes before and after LASIK.
References
1. Smiddy WE. Atypical presentations of macular holes. ArchOphthalmol 1993;111:62631.
2. Kokame GT. Early stage of macular hole in a severely myopiceye. Am J Ophthalmol 1995;119:2402.
3. Gass JD. Idiopathic senile macular hole. Its early stages andpathogenesis. Arch Ophthalmol 1988;106:62939.
4. Gass JD. Mller cell cone, an overlooked part of the anatomyof the fovea centralis: hypotheses concerning its role in thepathogenesis of macular hole and foveomacular retinoschisis.Arch Ophthalmol 1999;117:8213.
5. Pallikaris IG, Papatzanaki ME, Siganos DS, Tsilimbaris MK.A corneal flap technique for laser in situ keratomileusis:human studies. Arch Ophthalmol 1991;109:1699702.
6. Zaldivar R, Davidorf JM, Oscherow S. Laser in situ kerato-mileusis for myopia from 5.50 to 11.50 diopters withastigmatism. J Refract Surg 1998;14:1925.
7. Mulhern MG, Condon PI, OKeefe M. Endophthalmitis after
astigmatic myopic laser in situ keratomileusis. J CataractRefract Surg 1997;23:948 50.
8. Stulting RD, Carr JD, Thompson KP, et al. Complications oflaser in situ keratomileusis for the correction of myopia.Ophthalmology 1999;106:1320.
9. Kim HM, Jung HR. Laser assisted in situ keratomileusis forhigh myopia. Ophthalmic Surg Lasers 1996;27(suppl):S50811.
10. Ozdamar A, Aras C, Sener B, et al. Bilateral retinal detach-
ment associated with giant retinal tear after laser-assisted insitu keratomileusis. Retina 1998;18:176 7.
11. Ruiz-Moreno JM, Perez-Santonja JJ, Alio JL. Retinal detach-ment in myopic eyes after laser in situ keratomileusis. Am JOphthalmol 1999;128:58894.
12. Aras C, Ozdamar A, Karacorlu M, et al. Retinal detachmentfollowing laser in situ keratomileusis. Ophthalmic Surg Lasers2000;31:1215.
13. Farah ME, Hofling-Lima AL, Nascimento E. Early rhegmat-ogenous retinal detachment following laser in situ keratom-ileusis for high myopia. J Refract Surg 2000;16:73943.
14. Arevalo JF, Ramirez E, Suarez E, et al. Incidence of vitreo-retinal pathologic conditions 24 months after laser-assisted insitu keratomileusis. Ophthalmology 2000;107:258 62.
15. Arevalo JF, Ramirez E, Suarez E, et al. Rhegmatogenousretinal detachment after laser-assisted in situ keratomileusis(LASIK) for the correction of myopia. Retina 2000;20:33841.
16. Luna JD, Reviglio VE, Juarez CP. Bilateral macular hemor-rhage after laser in situ keratomileusis. Graefes Arch Clin ExpOphthalmol 1999;237:6113.
17. Ruiz-Moreno JM, Perez-Santonja JJ, Alio JL. Choroidal neo-vascularization in myopic eyes after laser-assisted in situkeratomileusis. Retina 2001;21:11520.
18. Chan CK, Lawrence FC II. Macular hole after laser in situkeratomileusis and photorefractive keratectomy. Am J Oph-thalmol 2001;131:6667.
19. Ruiz-Moreno JM, Artola A, Perez-Santonja JJ, Alio JL. Mac-ular hole in a myopic eye after laser in situ keratomileusis. J
Refract Surg 2002;18:746 9.20. Ruiz-Moreno JM, Alio JL. Incidence of retinal disease fol-
lowing refractive surgery in 9,239 eyes. J Refract Surg 2003;19:53447.
21. Arevalo JF, Mendoza AJ, Velez-Vazquez W, et al. Macularhole after LASIK [letter]. J Refract Surg 2004;20:85.
22. Morita H, Ideta H, Ito K, et al. Causative factors of retinaldetachment in macular holes. Retina 1991;11:2814.
23. Patel SC, Loo RH, Thompson JT, Sjaarda RN. Macular holesurgery in high myopia. Ophthalmology 2001;108:377 80.
24. Luna JD, Artal MN, Reviglio VE, et al. Vitreoretinal alter-ations following laser in situ keratomileusis: clinical and ex-perimental studies. Graefes Arch Clin Exp Ophthalmol 2001;239:41623.
25. Kakehashi A, Kado M, Akiba J, Hirokawa H. Variations ofposterior vitreous detachment. Br J Ophthalmol 1997;81:52732.
26. Oshima Y, Ikuno Y, Motokura M, et al. Complete epiretinalmembrane separation in highly myopic eyes with retinal de-tachment resulting from a macular hole. Am J Ophthalmol1998;126:66976.
27. Seike C, Kusaka S, Sakagami K, Ohashi Y. Reopening ofmacular holes in highly myopic eyes with retinal detachments.Retina 1997;17:2 6.
Ophthalmology Volume 112, Number 7, July 2005
1212
-
8/11/2019 B116ArevX12
12/20
Optical Coherence TomographyCharacteristics of Choroidal Metastasis
J. Fernando Arevalo, MD, FACS, Carlos F. Fernandez, MD, Reinaldo A. Garcia, MD
Purpose: To report 4 patients (7 eyes) with choroidal metastasis (primary: breast [2], lung [1], and unknown[1]) visualized with optical coherence tomography (OCT).
Design: Retrospective case series.Participants: Four patients (7 eyes) with choroidal metastasis participated in the study.Methods: Clinical examination, ultrasonography, fluorescein angiography, and OCT were performed in all cases.Main Outcome Measures: Optical coherence tomography characteristics.Results: Three patients suffered a gradual onset of blurred vision in both eyes. The fourth presented a
unilateral decrease in visual acuity. Bilateral choroidal lesions with various degrees of exudative retinal detach-ment (RD) were present in 3 of our 4 patients, and there was 1 case of a unilateral unifocal choroidal lesion.Optical coherence tomography revealed anterior displacement of the photoreceptor layer by subretinal fluid(hyporeflective space) overlying a hyperreflective thickened retinal pigment epitheliumchoriocapillaris complex.Subretinal deposits with several degrees of hyperreflectivity were seen, as well as loss of normal retinal
architecture with intraretinal splitting, identified as regions of low reflectance within the neurosensory retina. Afterchemotherapy, OCT demonstrated improvement of the serous RD and reduction of the lesions size withrecovery of the normal retinal architecture.
Conclusions: Optical coherence tomography in patients with choroidal metastasis allows evaluation ofsecondary retinalretinal pigment epithelial changes. In addition, the technique is useful in the follow-up oflesions after treatment. However, some limitations result from the choroidal location of the metastasis. Furtherstudies with clinicopathological correlation are needed to confirm our observations. Ophthalmology 2005;112:16121619 2005 by the American Academy of Ophthalmology.
Although intraocular metastases were historically considered arare finding,1,2 metastatic carcinoma to the choroid is nowrecognized as the most common intraocular neoplasm.36 In
contrast, metastasis limited to the retina and opticdisc remainsseldom, with only few reports in the literature.5 Clinical andhistopathological studies on choroidal metastasis have shown anumber of associated secondary changes in the overlying retinaand retinal pigment epithelium (RPE).6 In the past diagnosedonly at the time of enucleation or autopsy, more recentlyintraocular metastasis has been diagnosed in a clinical settingas a result of more comprehensive care of patients with carci-nomatosis, improved detection with diagnostic vitrectomy orvitreous aspiration, and increased survival time of patients withcancer.6
Optical coherence tomography (OCT) provides cross-sectional imaging of primarily the retina and RPE, withdeeper tissues, including the choroid and sclera, showing
poorer resolution. A study by Schaudig et al7 concludedthat, because the OCT beam is strongly scattered by theRPE, reflections from within the tumor mass are weak and,therefore, OCT is not useful for in vivo histological typingof choroidal tumors. However, there are some studies inwhich changes of the RPE and the neurosensory retina inpatients with choroidal melanoma were visualized byOCT.7,8 Optical coherence tomography may be useful tovisualize retinal complications associated with choroidaltumors, including choroidal hemangioma. In addition, OCTmay be useful to evaluate the response of choroidal tumorsto treatment. To our knowledge, there are no publishedstudies that assess the retinal changes associated with cho-
roidal metastasis; however, there is one report of metastaticbreast carcinoma to the retina confirmed by OCT.9
The objective of this report is to describe 4 cases ofchoroidal metastasis with changes of the RPE and the neu-rosensory retina confirmed by OCT.
Patients and Methods
Institutional review board/ethics committee approval was not re-quired for this study. A computer-based search of the ClnicaOftalmolgica Centro Caracas medical records was performed toidentify patients undergoing OCT evaluation for choroidal metas-
Originally received: November 13, 2004.
Accepted: March 17, 2005. Manuscript no. 2004-295.From the Retina and Vitreous Service, Clnica Oftalmolgica CentroCaracas, Caracas, Venezuela.
Presented in part at: American Academy of Ophthalmology Annual Meet-ing, October, 2004; New Orleans, Louisiana.
Supported in part by the Fundacin Arevalo-Coutinho para la Investigacinen Oftalmologa, Caracas, Venezuela (JFA, CFF, RAG), and the Pan-American Ophthalmological Foundation, Arlington, Texas (CFF).
The authors have no proprietary or financial interest in any products ortechniques described in the article.
Correspondence and reprint requests to J. Fernando Arevalo, MD, ClinicaOftalmolgica Centro Caracas, Centro Caracas PH-1, Av. Panten, SanBernardino, Caracas 1010, Venezuela. E-mail: [email protected].
1612 2005 by the American Academy of Ophthalmology ISSN 0161-6420/05/$see front matterPublished by Elsevier Inc. doi:10.1016/j.ophtha.2005.03.030
-
8/11/2019 B116ArevX12
13/20
Figure 1. Case 1.A, Choroidal metastasis associated with a perifoveolar serous retinal detachment (RD), and alterations in the retinal pigment epithelium
in the right eye.B, A choroidal tumor with an extensive serous RD in the left eye.C, Fluorescein angiography revealed late hyperfluorescence with areas
of hypofluorescence in the right eye. D, Fluorescein angiography showed no apparent contribution of the tumor in the left eye. E, B- and A-scan
ultrasonography showed a choroidal mass pattern with moderate internal reflectivity in the right eye.F
, B- and A-scan ultrasonography showed a choroidal
mass pattern with moderate internal reflectivity in the left eye with an exudative RD. dB decibels.
Table 1. Clinical Findings of 4 Patients (7 Eyes) with Choroidal Metastasis Visualized with Optical Coherence Tomography
PatientNo.
Age(yrs) Gender Eye(s)
Time betweenCancer Diagnosis
and Metastasis(mos)
Follow-up(mos)
PrimaryTumor
VisualAcuity
No. ofLesions
FindingsRightEye
LeftEye
RightEye
LeftEye Right Eye Left Eye
1 42 F Both 3 7 Lung 20/25 LP 1 2 CCT, SRD, CBP CYC, SRD2 47 F Both 24 6 Breast 20/32 20/80 1 2 CCT, SRD CCT, SRD3 77 F Both NA 2 Unknown HM CF 1 1 Uveitis, SRD,
SRP, SRESRD, SRP,
SRE, VH4 63 F Left 96 2 Breast 20/25 CF 0 1 CYC, SRD CYC, SRD
CBP clumps of brown pigment; CCT creamy choroidal tumor; CF counting fingers; CYC creamy yellow choroidal tumor; F female; HM hand movements; LP light perception; NA not available; SRD serous retinal detachment; SRE subretinal exudates; SRP subretinal pigment;VH vitreous hemorrhage.
1613
-
8/11/2019 B116ArevX12
14/20
tasis between May 1, 2003 and May 1, 2004. All patients wereevaluated in the practice of one of the authors (JFA). Opticalcoherence tomography was performed as previously described10
using a Zeiss OCT III instrument (Carl Zeiss, Inc., Dublin, CA)and version 3.0 software. Four patients (7 eyes) suffering fromchoroidal metastasis (primary: breast [2], lung [1], and unknown[1]) visualized with OCT were identified. Their clinical findingsare shown inTable 1.
Case Reports
Case 1
A 42-year-old female was referred for 2 months duration ofprogressive decrease of visual acuity (VA) in the left eye (LE). Hermedical history was significant for biopsy-proven lung adenocar-cinoma diagnosed three months earlier. She had no evidence ofmetastasis. Best-corrected VAs (BCVAs) were 20/25 (right eye)and light perception (left eye). Intraocular pressures (IOPs) were14 mmHg (right eye) and 30 mmHg (left eye). Anterior segmentexamination was unremarkable in her right eye. In the left eye, shehad fine keratic precipitates, 1 cells and flare in the anteriorchamber, rubeosis iridis, and 3 anterior vitreous cells. Fundusexamination of the right eye showed an inferotemporal juxtafo-veolar dome-shaped creamy choroidal tumor associated with aperifoveolar serous retinal detachment (RD) and alterations in theRPE (clumps of brown pigment on the surface of the tumor) ( Fig1A). A creamy yellow choroidal tumor with an extensive serousRD that involved the macula was seen in the left eye (Fig 1B).Fluorescein angiography (FA) revealed that the choroidal tumorshowed late hyperfluorescence in the right eye (Fig 1C), and thechoroidal involvement was masked during FA in the left eye by theextensive exudative RD (Fig 1D). B-scan ultrasonography showeda choroidal mass with high acoustic solidity, and the A scanshowed moderate internal reflectivity in both eyes (Fig 1E, F), witha high-intensity linear echo characteristic of an RD in the left eye(Fig 1F). Optical coherence tomography examination of the righteye showed a dome-shaped elevation of a normal retina attached tothe RPEchoriocapillaris complex (Fig 2A) and a region of lowreflectance corresponding to a neurosensory detachment. In addi-
tion, OCT demonstrated highly reflective points inside the neuro-sensory retina, which may correspond to retinal compromise bycancer cells or inflammatory cells; a double highly reflective bandat the RPEchoriocapillaris complex; shadowing in some parts ofthe RPE choriocapillaris complex; increased thickness of theRPEchoriocapillaris complex (Fig 2B); and intraretinal splitting,identified as regions of low reflectance within the neurosensoryretina (Fig 2C).
Case 2
A 47-year-old female was referred to us for 2 weeks duration ofprogressive decrease of VA in both eyes. A significant aspect ofher medical history was a diagnosis for breast cancer 2 yearsearlier. She had no evidence of metastasis. Her BCVAs were 20/32(right eye) and 20/80 (left eye). Intraocular pressures were 14mmHg (right eye) and 11 mmHg (left eye). Anterior segmentexamination was unremarkable in both eyes. Fundus examinationof the right eye showed a superotemporal dome-shaped creamychoroidal tumor associated with a serous RD and an inferotempo-
Figure 2. Case 1.A, Optical coherence tomography examination (black cross
inFig 1A) of the right eye showed a dome-shaped elevation of the normal retina
attached to the retinal pigment epithelium (RPE)choriocapillaris complex (ar-
row). B, A regionof lowreflectance corresponding to a neurosensory detachment,
highly reflective points inside the neurosensory retina perhaps corresponding to
retinal compromise by cancer cells or inflammatory cells (arrow), a double highly
reflective band at the RPEchoriocapillaris complex, shadowing in some parts of
the RPEchoriocapillaris complex (arrowhead), and increased thickness of the
RPEchoriocapillaris complex. C, Intraretinal splitting, identified as regions of
low reflectance within the neurosensory retina (arrow).
3
Figure 3. Case 2. A, A superotemporal dome-shaped creamy choroidal tumor associated with a serous retinal detachment (RD) in the right eye.B, An
inferotemporal dome-shaped creamy choroidal tumor associated with a serous RD in the macular area of the left eye. C, Fluorescein angiography in the
right eye without apparent changes. D, A choroidal tumor showed late hyperfluorescence in the macular area and nasal quadrant of the left eye, with
pinpoint foci of hyperfluorescence over the tumor.E, F, B- and A-scan ultrasonography showed a choroidal mass pattern with high acoustic solidity in
both eyes. A-scan ultrasonography showed moderate internal reflectivity in both eyes.
Ophthalmology Volume 112, Number 9, September 2005
1614
-
8/11/2019 B116ArevX12
15/20
Arevalo et al OCT and Choroidal Metastasis
1615
-
8/11/2019 B116ArevX12
16/20
ral creamy yellow choroidal tumor with a serous RD that involvedthe macula in the left eye (Fig 3A, B). There was no apparentcontribution of the choroidal tumor evident with FA in the righteye (Fig 3C). Fluorescein angiography revealed late hyperfluores-cence in the macular area and nasal quadrant of the left eye, withpinpoint foci of hyperfluorescence over the tumor (Fig 3D). B-scanultrasonography showed a choroidal mass pattern with high acous-tic solidity, and the A scan showed moderate internal reflectivity inboth eyes (Fig 3E, F). Optical coherence tomography of the right
eye showed a low reflectance elevation of the macular region,corresponding to a neurosensory detachment (Fig 4A); an increasein thickness of the RPEchoriocapillaris complex (Fig 4B, C); andfocal elevation of the retina with subretinal hyperreflectivity (Fig4C). In the left eye, OCT showed low reflectance in the macularregion, corresponding to a neurosensory RD (Fig 5A); a highlyreflective lesion overlying the RPEchoriocapillaris complex;thickening of the retina with hyporeflective areas in the subretinalspace (Fig 5B); and intraretinal splitting, identified as a region oflow reflectance within the neurosensory retina (Fig 5C). Afterchemotherapy, OCT showed improvement of the serous RD and areduction in the size of the lesion, with recovery of the normalretinal architecture in both eyes (Figs 6, 7).
Case 3A 77-year-old female was referred to our clinic because of pro-gressive decrease in VA of 6 months duration in both eyes. Hermedical history was unremarkable. Her BCVAs were hand move-ments (right eye) and counting fingers (CF) (left eye). Intraocularpressures were 8 mmHg (right eye) and 12 mmHg (left eye).Anterior segment examination revealed nuclear sclerosis in botheyes and 2 cells and flare in the anterior vitreous in the right eye.Fundus examination showed vitreitis in the right eye and serousRD in both eyes, with subretinal precipitates, exudates, and vitre-ous hemorrhage in the left eye. On FA, the choroidal tumorshowed late hyperfluorescence in the macular area in both eyes.B-scan ultrasonography showed a lowinternal reflectivity dome-shaped mass and high-intensity linear echo characteristic of an RD
in both eyes. Optical coherence tomography showed a low-reflec-tance macular region corresponding to a neurosensory detachment,loss of normal retinal architecture, highly reflective points overly-ing the RPEchoriocapillaris complex, an increase in thickness ofthe RPEchoriocapillaris complex, and a highly reflective lesionoverlying the RPEchoriocapillaris complex in the right eye. Inthe left eye, OCT showed a low-reflectance macular region corre-sponding to a neurosensory detachment, a highly reflective lesionoverlying the RPEchoriocapillaris complex, loss of normal reti-nal architecture, and an increase in the RPEchoriocapillaris com-plex thickness cystic changes. A clinical diagnosis of choroidal
metastasis was made, and a systemic workup was ordered. How-ever, the patient has been lost to follow-up.
Case 4
A 63-year-old female had a medical history significant for breastcancer diagnosed 8 years earlier and evidence of liver metastasis of2 years duration treated with radiotherapy and 6 sessions ofchemotherapy. She was referred to our clinic with a diagnosis of an
RD with an underlying mass in her left eye. Her BCVAs were20/25 (right eye) and CF (left eye). The IOP was 10 mmHg in botheyes. The anterior segment examination was unremarkable, andshe had an intraocular lens in both eyes. Fundus examination of theright eye was normal. The left eye showed a central dome-shapedcreamy yellow choroidal tumor with clumps of brown pigment onthe surface of the tumor, associated with a serous RD that involvedthe macula(Fig 8A). Fluorescein angiography revealed early hy-perfluorescence of the disc and hypofluorescence of the mass withleopard spots. Optical coherence tomography showed (1) an in-crease in thickness and detachment of the RPEchoriocapillariscomplex associated with highly reflective deposits correspondingto the leopard spots and the elevated choroidal mass (Fig 8B); (2)low reflectance of the macular region, corresponding to an exuda-tive RD; and (3) neurosensory retinal atrophy.
Discussion
Choroidal metastasis may cause secondary retinal changes.There is little information on the OCT appearance of thesesecondary changes. The aim of this report was therefore todemonstrate the appearance of secondary retinal changes as-sociated with choroidal metastasis when imaged with OCT.Metastatic cancer to the uvea and optic disc involves theposterior pole in 40% of cases.6 This allowed us to performOCT examination of these lesions. However, for lesionsthicker than 2 mm, it is impossible to have both the base and
the surface of the tumor on the same scan. Therefore, measur-ing the height of larger lesions with OCT is not possible.Shields et al11 examined 520 eyes with uveal metastasis andfound that breast cancer choroidal metastasis had the strongesttendency to occur as a multifocal and bilateral tumor, and thatmost choroidal metastases were plateau or dome shaped andmeasured approximately 3 mm in thickness. Thicker tumorsgenerally were observed with metastasis originating from thegastrointestinal tract, kidney, lung, and prostate. However,breast cancer metastases showed a tendency toward flatter
3
Figure 4. Case 2.A, Optical coherence tomography in the right eye (black cross inFig 3A) showed low reflectance in the macular region, correspondingto a neurosensory detachment (arrow).B, An increase in thickness of the retinal pigment epithelium (RPE)choriocapillaris complex (arrow) and an
intraretinal highly reflective spot with RPEchoriocapillaris complex shadowing posteriorly (arrowhead) C, Focal elevation of the retina with subretinal
hyperreflectivity and hyporeflectivity (arrows).
Figure 5. Case 2. Optical coherence tomography in the left eye. A, Low reflectance in the macular region (black cross in Fig 3B), corresponding to a
shallow neurosensory retinal detachment (arrow), and retinal pigment epithelium (RPE)choriocapillaris complex hyperreflectivity. B, A highly reflective
lesion overlying the RPE choriocapillaris complex (arrow) and thickening of the retina with hyporeflective areas in the subretinal space (arrowhead).C,
Intraretinal splitting, identified as a region of low reflectance within the neurosensory retina (arrow).
Figure 6. Case 2. Optical coherence tomography of the right eye after chemotherapy. A, Improvement in the macular serous retinal detachment. B,
Reduction of the lesions, with recovery of the normal retinal architecture.
Figure 7. Case 2. Optical coherence tomography of the left eye after chemotherapy. A, Improvement in the macular serous retinal detachment. B,
Reduction of the lesions with recovery of the normal retinal architecture. Atrophy of the retinal pigment epithelium was greater in this eye, with higher
reflectivity scattered from the choroid as compared with the right eye (arrow).
Ophthalmology Volume 112, Number 9, September 2005
1616
-
8/11/2019 B116ArevX12
17/20
Arevalo et al OCT and Choroidal Metastasis
1617
-
8/11/2019 B116ArevX12
18/20
tumors, having a mean thickness of only 2 mm in the largest
tumor focus.Clinical and histopathological studies of patients with cho-
roidal tumors have shown that common associated secondarychanges include serous RD extending beyond the limit of thetumor, atrophy of the RPE, atrophy of the retina starting in thephotoreceptor layer, cystoid retinal degeneration leading toretinoschisis, and invasion of the sensory retina by the tu-mor.6,12 Optical coherence tomography cannot give any invivo information on the histology of choroidal tumors; how-ever, this imaging technique can clearly show retinal changesin the tissue surrounding and overlying the choroidal tumor.7,8
In our report, OCT revealed low-reflectance regions corre-
sponding to neurosensory RD (85.7%), highly reflective le-sions overlying the RPEchoriocapillaris complex (85.7%), athickened retinal RPEchoriocapillaris complex (71.4%),highly reflective points in the subretinal space (14.2%), andloss of normal retinal architecture with highly reflective pointsinside the neurosensory retina (28.5%). In addition, intraretinalsplitting, identified as regions of low reflectance within theneurosensory retina, was observed (28.5%). These character-
istics lead us to question whether or not the retina is compro-mised with malignant cells and should be correlated withclinical findings. Furthermore, OCT may help in diagnosis,determination of disease extension, and evaluation after treat-ment, as demonstrated in our case 2.
The interpretation of our results is difficult without his-topathologic correlation. The high rate of neurosensory RDand RPE alterations is in concordance with Shields et al,11 whoreported associated subretinal fluid (SRF) in 73% of their 520eyes with uveal metastases and RPE alterations in 57%. In-traretinal splitting could have been simply a result of chronicityor a consequence of the aggressive nature of the tumor. Somemetastatic tumors develop ophthalmoscopically visible indi-
vidual nodules or tumor cells on the apex of the tumor andunder Bruchs membrane. This observation should not beinterpreted as a break in Bruchs membrane. However, withOCT we found a rupture of the RPE choriocapillaris complex.The highly reflective points inside the neurosensory retina andin the subretinal space may correspond to retinal compromiseby cancer cells or macrophages containing lipofucsin andmelanin granules.6 After chemotherapy, OCT of our case 2showed improvement of the serous RD and reduction of thelesions size, with recovery of the normal retinal architecture inboth eyes. Small changes in tumor prominence could be ob-
jectivelymeasured with OCT and interpreted as signs of pro-gression.7
Truong et al,9 in their case report of metastatic breastcarcinoma to the retina visualized by OCT, found a highlyreflective lesion within the retina, with associated neurosen-sory detachment in the temporal portion of the fovea and noapparent connection to the choroid. No abnormalities oftheRPE or choriocapillaris were visualized. Muscat et al8 re-ported secondary retinal changes associated with choroidalnevi and melanomas documented by OCT. Both studiesconcluded that OCT helped demonstrate that the lesion wasconfined to the retina, without involvement of the underly-ing RPE or choriocapillaris, and that the secondary retinalchanges were associated with choroidal lesions. Recently,Espinoza et al13 used OCT in the evaluation of retinalchanges associated with suspicious choroidal melanocytic
tumors. They concluded that OCT is useful in distinguish-ing active SRF from chronic retinal changes overlying achoroidal melanocytic tumor, and that OCT findings mayhave predictive value in identifying tumors that are likely togrow and require treatment.
One of the limitations of our study is that, as we had onlya small number of patients and there was no histopathologiccorrelation, the conclusions are not generalizable to allchoroidal metastases. In addition, in one of our cases theprimary tumor was unknown. However, Shields et al11
report that up to half of these patients will not have aprimary site detected, despite systemic evaluation by med-
Figure 8. Case 4. A, Fundus examination of the left eye showed a central
dome-shaped creamy-yellow choroidal tumor with clumps of brown pigment
on its surface, associated with a serous retinal detachment that involved the
macula. B, Optical coherence tomography (black line on A) showed an
increase in thickness and detachment of the retinal pigment epithelium
choriocapillaris complex associated with highly reflective deposits (arrow),
corresponding to the leopard spots and the elevated choroidal mass.
Ophthalmology Volume 112, Number 9, September 2005
1618
-
8/11/2019 B116ArevX12
19/20
ical oncologists, and many ultimately die of disseminatedmetastatic disease, with the primary site remaining un-known. In our study, our patient with metastatic diseasewith the primary site unknown was lost to follow-up.
In summary, OCT is a useful imaging technique to studychoroidal metastatic tumors. Optical coherence tomographyin patients with choroidal metastasis demonstrates the sec-ondary retinaRPE changes. In addition, OCT is useful in
follow-up of lesions after treatment. However, OCT imag-ing is limited by the choroidal location of metastasis. Fur-ther studies with clinicopathological correlation are neededto confirm our observations.
References
1. Duke-Elder S, Perkins ES. Diseases of the uveal tract. In:Duke-Elder S, ed. System of Ophthalmology. Vol. 9. St.Louis: Mosby; 1966:91737.
2. Ferry AP. Metastatic carcinoma of the eye and ocular adnexa.Int Ophthalmol Clin 1967;7:61558.
3. Duke JR, Walsh FB. Metastatic carcinoma to the retina. Am J
Ophthalmol 1959;47:448.4. Koenig RP, Johnson DL, Monahan RH. Bronchogenic carci-
noma with metastases to the retina. Am J Ophthalmol 1963;56:8279.
5. Leys AM, Van Eyck LM, Nuttin BJ, et al. Metastatic carci-noma to the retina: clinicopathologic findings in two cases.Arch Ophthalmol 1990;108:144852.
6. Shields JA, Shields CL. Intraocular Tumors: A Text and Atlas.Philadelphia: WB Saunders; 1992:20738.
7. Schaudig U, Hassenstein A, Bernd A, et al. Limitations ofimaging choroidal tumors in vivo by optical coherencetomography. Graefes Arch Clin Exp Ophthalmol 1998;236:58892.
8. Muscat S, Parks S, Kemp E, Keating D. Secondary retinalchanges associated with choroidal naevi and melanomas doc-umented by optical coherence tomography. Br J Ophthalmol2004;88:1204.
9. Truong SN, Fern CM, Costa DL, Spaide RF. Metastatic breastcarcinoma to the retina: optical coherence tomography find-ings. Retina 2002;20:8135.
10. Puliafito CA, Hee MR, Lin CP, et al. Imaging of maculardiseases with optical coherence tomography. Ophthalmology1995;102:21729.
11. Shields CL, Shields JA, Gross NE, et al. Survey of 520 eyeswith uveal metastases. Ophthalmology 1997;104:126576.
12. Damato BE, Foulds WS. Tumour-associated retinal pigmentepitheliopathy. Eye 1990;4:3827.
13. Espinoza G, Rosenblatt B, Harbour JW. Optical coherencetomography in the evaluation of retinal changes associatedwith suspicious choroidal melanocytic tumors. Am J Ophthal-mol 2004;137:905.
Arevalo et al OCT and Choroidal Metastasis
1619
-
8/11/2019 B116ArevX12
20/20
Arevalo et al. Trabajos Cientificos/Handout/Pg. 1
Suggested Reading
1. Cartwright VA, McGhee CN. Ophthalmology and vision science research. Part 1:Understanding and using journal impact factors and citation indices.
J Cataract Refract Surg. 2005 Oct;31(10):1999-2007.
2. McGhee CN, Gilhotra AK. Ophthalmology and vision science research: part 2: How
to commence research--Eureka or that's a little unusual? J Cataract Refract Surg. 2005
Nov;31(11):2205-11.
3. McGhee CN, Gilhotra AK. Ophthalmology and vision science research: Part 3:avoiding writer's block--understanding the ABCs of a good research paper.
J Cataract Refract Surg. 2005 Dec;31(12):2413-9.
4. Gilhotra AK, McGhee CN. Ophthalmology and vision science research. Part 4:avoiding rejection--structuring a research paper from introduction to references. J
Cataract Refract Surg. 2006 Jan;32(1):151-7.
5. Sherwin T, Gilhotra AK. Ophthalmology and vision science research: part 5: surfingor sieving--using literature databases wisely. J Cataract Refract Surg. 2006
Feb;32(2):334-40.
6. Jabs DA. Improving the reporting of clinical case series.
Am J Ophthalmol. 2005 May;139(5):900-5.
7. Beck RW. Sample size for a clinical trial: why do some trials need only 100 patients
and others 1000 patients or more? Ophthalmology. 2006 May;113(5):721-2.
8. DiLoreto DA Jr, Bressler NM, Bressler SB, Schachat AP. Use of best and final visual
acuity outcomes in ophthalmological research. Arch Ophthalmol. 2003
Nov;121(11):1586-90.
9. Schachat AP, Chambers WA, Liesegang TJ, Albert DA. Safe and effective.Ophthalmology. 2003 Nov;110(11):2073-4.
10. STUDY DESIGN WORKSHEETS. The study design worksheets are intended as guidelines oforganization of manuscripts and to aide the consistency and quality of peer review. The only worksheet
which is mandatory is the Consort Agreement for a Randomized Controlled Trial (see Ophthalmology2003;110:225-27). All other study design worksheets are optional and available at our websiteor see
Ophthalmology 2003;110:227-44 .
http://www.elsevier.com/framework_products/promis_misc/620418forms.htmhttp://www.elsevier.com/framework_products/promis_misc/620418forms.htm