HDMICS Koutsiaris 2016
Click here to load reader
-
Upload
koutsiaris-aris -
Category
Documents
-
view
34 -
download
0
Transcript of HDMICS Koutsiaris 2016

AU
THO
R C
OP
Y
Clinical Hemorheology and Microcirculation 61 (2015) 429–438DOI 10.3233/CH-141888IOS Press
429
Correlation of axial blood velocity to venularand arteriolar diameter in the human eyein vivo
Aristotle G. Koutsiaris∗
Bio-Medical Informatics Laboratory, Department of Medical Laboratories, School of Health Sciences,Technological Educational Institute (TEI) of Thessaly, Larissa, Greece
Abstract. The axial blood velocity (Vax) association with microvessel diameter (D) was studied at 104 different postcapillaryvenules (4 �m < D < 24 �m) and 30 different precapillary arterioles (6 �m ≤ D ≤ 12 �m) in the human conjunctiva of normalhealthy humans. Venular diameter sizes were classified as “very small” (Group 1, 4.4 �m ≤ D < 8.9 �m), “small” (Group 2,8.9 �m ≤ D < 13.8 �m), “medium” (Group 3, 13.8 �m ≤ D < 19.1 �m) and “large” (Group 4, 19.1 �m ≤ D ≤ 23.5). The Spear-man’s correlation coefficient (rs) in all 4 venular groups was less than 0.36 and not statistically significant (n = 26, p ≥ 0.08).Similar correlation results were observed for the arteriolar group (rs) ≈ 0) for the peak systolic, the average and the end systolicaxial velocities. Vax was significantly (p < 0.001) lower in Group 1 in comparison to that in Group 2 and significantly (p < 0.01)lower in Group 2 in comparison to that in Group 3. However, Vax was not significantly lower in Group 3 in comparison to thatin Group 4. Average Vax and standard deviation was 0.48 ± 0.13, 0.64 ± 0.16, 0.82 ± 0.25 and 0.88 ± 0.32 mm/s for Groups1, 2, 3 and 4 respectively. The above results reinforce the importance of measuring D in microvascular hemodynamics. Higherdiameters suggest higher axial velocities but Vax does not change significantly within the limits of each of the aforementionedgroups.
Keywords: Human, eye, conjunctiva, venules, arterioles, axial velocity, diameter, correlation
1. Introduction
Blood velocity measurements in the human smallest microvessels appeared in the seventies [3, 4, 10].Since then, several groups published velocity measurements from various human tissues such as the nailfold [24, 28, 29, 34], the bulbar conjunctiva [6, 12, 13, 18, 20, 32] and the retina [1, 23, 30, 35].
In the majority of the above cases the quantity that was actually measured was the axial or centerlineblood velocity (Vax). However, the relationship of Vax to micro vessel diameter has not been studied indetail, in humans. In fact, many of the researchers did not report diameter measurements in relation tothe measured Vax [1, 13, 23, 30, 34].
In general, in mammal microcirculation, higher diameters suggest higher velocities but this generalprinciple does not seem to be valid for small variations of diameter [16]. The question that has not beenanswered yet is how “small” these diameter variations might be and answering this question for humanswas one of the targets of this work.
∗Corresponding author: Dr. Aristotle Koutsiaris, 9 Miauli St, 41223 Larissa, Greece. Tel.: +30 2410 411284; E-mails:[email protected]; [email protected].
1386-0291/15/$35.00 © 2015 – IOS Press and the authors. All rights reserved

AU
THO
R C
OP
Y
430 A.G. Koutsiaris / Correlation of axial blood velocity to venular and arteriolar diameter
If a monotonic association between Vax and D does not exist or, if it is weak and not statisticallysignificant, at a specific diameter range, then all velocity measurements in that range could be treated asone group or cluster. Therefore, another target of this work was to give average values of Vax of healthyindividuals in correspondence to specific diameter ranges. This could be proved useful to other exper-imental investigations and to other groups developing new semi-automatic or fully automatic velocitymeasurement techniques.
In addition, it could have a clinical or diagnostic application. For example, conjunctival Vax has beenused to discriminate sickle cell disease patients [6], Alzheimer’s disease patients [27] and Type-1 diabetesmellitus patients [7].
Also, statistically significant differences in the Vax of the conjunctival microcirculation have beenreported after the application of contact lenses [8, 12] and transfusion therapy [9].
Other important hemodynamic parameters which can be estimated from Vax are volume flow Q [17],wall shear stress WSS [18, 21], the velocity profile [19] and the resistive index RI [20, 22].
All the above parameters are essential in many research areas such as theoretical models on vasculardesign [15], the amount of chemicals exchanged between blood and tissue, the micro mechanobiologyof endothelium cells in health and disease and vascular targeted drug carriers [5].
Furthermore, hemodynamic parameters are important for the realistic design of in vitro apparatusesand assays for the study of angiogenesis [14], the blood brain barrier [25], the endothelial response [11,31] and cell adhesion. Cell adhesion is a broad topic implicated in many research areas comprising theattachment of circulating tumor cells, tissue engineering and regenerative medicine [33].
2. Methods
This work was carried out using previously measured velocity data [18, 20]. However, data statisticalprocessing, results and conclusions are all new.
2.1. Experimental set up
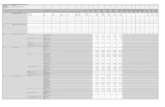
The experimental set up (Fig. 1) consisted of a slit lamp (Nikon FS-3 V) connected with a high-speedCCD camera (12 bit, PCO Computer Optics GmbH, Germany) and a PC (Pentium 4, 3 GHz). The systemproduced digital images of 320 × 240 pixels at a frame rate of 96 frames per second (fps) with an enhancedmaximum magnification of 242x and a digital resolution of 1.257 ± 0.004 �m/pixel.
2.2. Subjects
Images were taken from the venules of the right eyes (temporal side of the bulbar conjunctiva) of 17normal human volunteers (8 men and 9 women) and from the arterioles of the right eyes (temporal sideof the bulbar conjunctiva) of 15 normal human volunteers (9 men and 6 women).
The age of the 17 human volunteers for venular measurements ranged between 25 and 38 years with anaverage body mass index (BMI, defined as the number of body kilograms over the square of the height)of 24 ± 3 Kg/m2. All volunteers contributed by approximately the same number of velocity points (5 to7) to the total sample and from the total velocity point ensemble, 54 points were from females and 50points were from males.

AU
THO
R C
OP
Y
A.G. Koutsiaris / Correlation of axial blood velocity to venular and arteriolar diameter 431
Fig. 1. Experimental set-up.
The age of the 15 human volunteers for arteriolar measurements ranged between 24 and 38 years withan average BMI of 23 ± 3 Kg/m2. No volunteer contributed by more than two microvessels to the totalsample.
The individuals had no ocular or systemic disease, no smoking or alcohol habit and were not under anymedication. Recordings were not taken into account when a 25% (or more) change occurred in either ofthe initial systolic or diastolic arterial blood pressure. In addition, subjects with a diastolic blood pressuregreater than 95 mmHg were excluded from the study as hypertensive.
Data from female subjects were acquired after their menstruation and before the premenstrual periodof 8 days. All measurements were performed in a temperature controlled environment (21 to 24◦C) afterwaiting a predetermined time interval for adaptation. The project was approved by the research ethicscommittee of the university hospital of Larissa and informed consent was obtained from all participantsin the study.
2.3. Internal diameter (D) and axial velocity (Vax) measurement
The internal diameter (D) was estimated using the Pythagoras’s theorem from the coordinates of theintersection points between a vertical line to the vessel axis and the outer limits of the erythrocyte column.The diametrical value assigned to each arteriole was the average of 3 or 4 different measurements.
Axial erythrocyte velocity (Vax) was measured using the axial distance DC travelled by a RBC or aplasma gap, over a fixed time interval �t, where �t was known from the frame rate of the camera asequal to 10.04 ms.
2.4. Statistical analysis
The Microsoft Office EXCEL 2003 (professional edition) and the SOFA (version 1.4, Paton-Simpson& Associates Ltd) software were used for statistical analysis.
The 25th, 50th (median) and 75th percentiles, corresponding to venular diameters of 8.9, 13.8 and19.1 �m respectively, were selected as discriminators for classifying venular sizes as “very small”

AU
THO
R C
OP
Y
432 A.G. Koutsiaris / Correlation of axial blood velocity to venular and arteriolar diameter
(Group 1, 4.4 �m ≤ D < 8.9 �m), “small” (Group 2, 8.9 �m ≤ D < 13.8 �m), “medium” (Group 3,13.8 �m ≤ D < 19.1 �m) and “large” (Group 4, 19.1 �m ≤ D≤23.5).
The majority of the variable distributions were not normal and therefore differences between vesselgroups were examined using the Mann-Whitney U test. Spearman’s rank correlation coefficient (rs) wasused for measuring the strength of monotonic association between D and Vax. The level of significancewas set at p < 0.05.
3. Results
Venular diameters ranged between 4 and 24 �m and venular axial velocities between 0.24 and1.70 mm/s. Venular velocity points are shown as black dots in Fig. 2a. In the same figure, velocitypoints were grouped by vessel size into four venular groups with 26 points each, without overlappingdiameters, according to the Methods section.
The Spearman’s correlation coefficient (rs) for the 4 venular groups was less than 0.36 and notstatistically significant (n = 26, p ≥ 0.08) as it is shown in Table 1.
Descriptive statistics of D and Vax are shown in Tables 2, 3 and 4 for all four venular groups. The rangeof diameters for all vessel groups was between 4.4 and 5.1 �m. D and Vax were significantly (p < 0.001)lower in Group 1 in comparison to those in Group 2 (Table 2) and significantly (p < 0.01) lower in Group2 in comparison to those in Group 3 (Table 3). However, Vax was not significantly lower in Group 3 incomparison to that in Group 4 (Table 4).
In Fig. 2b, axial velocity average and standard deviation values are shown for each venular ves-sel group, namely 0.48 ± 0.13, 0.64 ± 0.16, 0.82 ± 0.25 and 0.88 ± 0.32 mm/s for Group 1, 2, 3 and 4respectively.
Finally, at the arteriolar side of the human bulbar conjunctiva, arteriolar diameters ranged between 6and 12 �m and arteriolar axial velocities between 0.40 and 5.84 mm/s, as it is shown in Fig. 3. Therewas practically no monotonic association (rs ≈ 0) between axial velocity and arteriolar diameter. Thiswas true for either the peak systolic (ARTPSV), the average (ARTAVV) and the end systolic (ARTEDV)axial velocities.
4. Discussion
The human eye is an open window to the human microcirculation and in most of the ophthalmologydepartments there are instruments with which operators can see blood flow. With some modifications, thesame instruments can be used to acquire image data appropriate for hemodynamic and morphologicalquantification [6, 12, 18, 26].
The most frequently measured hemodynamic parameters in the microcirculation are vessel diameterand axial blood velocity but not always in relation to one another.
In this work, conjunctival venules were categorized into four (4) groups by diameter and, investigatingVax in relation to D inside the limits of each group, it was found that there was no monotonic association(and consequently no correlation) between axial velocity and diameter.
The same was observed for the arteriolar group and it is furthermore supported by earlier recordingsfrom rabbit mesenteric precapillary arterioles [16]. Vax measurements from a total of 19 mesentericprecapillary arterioles ranging in diameter between 7.4 and 12.4 �m are shown in Fig. 4. Measurementsfrom 9 more precapillary arterioles are presented here in addition to those from 10 arterioles published

AU
THO
R C
OP
Y
A.G. Koutsiaris / Correlation of axial blood velocity to venular and arteriolar diameter 433
Fig. 2. (a) Blood axial velocity (Vax) measurements versus diameter (D) in the postcapillary venules of the human bulbarconjunctiva are shown as black dots. The 25th, 50th (median) and 75th percentiles, corresponding to venular diameters of 8.9,13.8 and 19.1 �m respectively, were selected as discriminators for classifying venular sizes as “very small” (Group 1), “small”(Group 2), “medium” (Group 3) and “large” (Group 4). (b) Average Vax and standard deviation for each group are shown inblack columns and black bars respectively.
Table 1
The Spearman’s correlation coefficient (rs ) for each of the 4 venular groups was weak (≤0.35) and not statisticallysignificant (n = 26, p > 0.08)
Vessel group rs P-value
Group 1 0.22 0.27Group 2 0.35 0.08Group 3 0.21 0.31Group 4 0.26 0.19

AU
THO
R C
OP
Y
434 A.G. Koutsiaris / Correlation of axial blood velocity to venular and arteriolar diameter
Table 2
Statistics of diameter (D) and axial velocity (Vax) measurements in venular Group 1 and Group 2. The number of venules inboth groups was equal to 26. Axial velocities in the two venular groups were significantly (p < 0.001) different
Statistics D (�m) Vax (mm/s)
Group 1 Group 2 Group 1 Group 2
Minimum 4.4 8.9 0.24 0.35Maximum 8.8 13.7 0.73 0.96Range 4.4 4.8 0.49 0.61Mean ± SD∗ 6.5 ± 1.3 11.2 ± 1.5 0.48 ± 0.13 0.64 ± 0.16Median 6.4 11.2 0.46 0.62P-value∗∗ <0.001 <0.001
∗Standard deviation, ∗∗Mann-Whitney U test.
Table 3
Statistics of diameter (D) and axial velocity (Vax) measurements in Group 2 and Group 3. The number of venules in bothgroups was equal to 26. Axial velocities in the two venular groups were significantly (p < 0.01) different
Statistics D (�m) Vax (mm/s)
Group 2 Group 3 Group 2 Group 3
Minimum 8.9 13.8 0.35 0.53Maximum 13.7 18.9 0.96 1.56Range 4.8 5.1 0.61 1.03Mean ± SD∗ 11.2 ± 1.5 16.2 ± 1.5 0.64 ± 0.16 0.82 ± 0.25Median 11.2 16.1 0.62 0.72P-value∗∗ <0.001 <0.01
∗Standard deviation. ∗∗Mann-Whitney U test.
Table 4
Statistics of diameter (D) and axial velocity (Vax) measurements in Group 3 and Group 4. The number of venules in bothgroups was equal to 26. Even though venular diameters were significantly (p < 0.001) different, axial velocities in the two
venular groups were not significantly (p = 0.69) different
Statistics D (�m) Vax (mm/s)
Group 3 Group 4 Group 3 Group 4
Minimum 13.8 19.1 0.53 0.43Maximum 18.9 23.5 1.56 1.70Range 5.1 4.4 1.03 1.27Mean ± SD∗ 16.2 ± 1.5 21.1 ± 1.3 0.82 ± 0.25 0.88 ± 0.32Median 16.1 21.0 0.72 0.82P-value∗∗ <0.001 0.69
∗Standard deviation. ∗∗Mann-Whitney U test.

AU
THO
R C
OP
Y
A.G. Koutsiaris / Correlation of axial blood velocity to venular and arteriolar diameter 435
Fig. 3. Blood axial velocity (Vax) versus diameter (D) in the precapillary arterioles of the human bulbar conjunctiva. ARTeriolarPeak Systolic Velocities (ARTPSV) are shown as rhombuses, ARTeriolar AVerage Velocities (ARTAVV) are shown as blackdots and ARTeriolar End Diastolic Velocities (ARTEDV) are shown as crosses. In all cases, there was no statistically significantmonotonic association (rs ≈ 0, p > 0.5).
Fig. 4. Blood axial velocity (Vax) versus diameter (D) in the precapillary arterioles of the rabbit mesentery. ARTeriolar PeakSystolic Velocities (ARTPSV) are shown as rhombuses, ARTeriolar AVerage Velocities (ARTAVV) are shown as black dotsand ARTeriolar End Diastolic Velocities (ARTEDV) are shown as crosses. In all cases, there was no statistically significantmonotonic association (0.13 ≤ rs ≤ 0.41, p ≥ 0.08).
previously [16]. There was no statistically significant (p ≥ 0.08) monotonic association between arteriolarvelocity and diameter for either the peak systolic (ARTPSV), the average (ARTAVV) and the end systolic(ARTEDV) values.
The above two paragraphs lead to a useful conclusion concerning axial blood velocity, that for venulardiameter spans less than ≈ 5 �m (Fig. 2a) and for arteriolar diameter spans less than ≈ 6 �m (Fig. 3),there is practically no correlation between Vax and D.

AU
THO
R C
OP
Y
436 A.G. Koutsiaris / Correlation of axial blood velocity to venular and arteriolar diameter
The next step was to compare the axial velocities from the 4 different venular groups. A statisticallysignificant difference among axial velocities in the first three groups (Tables 2 and 3) was found, indicatingthe importance of vessel diameter as a parameter influencing the value of axial velocity. This should betaken into account, especially when using instruments and techniques for measuring velocity in highdiameter spans, for example between 4 and 40 �m [23].
The results shown in Table 3 for Groups 2 and 3 are in accordance with Wanek et al. [32] who founda statistically significant difference between axial velocities measured in venules categorized into twogroups by vessel size using the diameter of 15 microns as a discriminator.
The average velocities of each of the 4 venular groups (Fig. 2b), might be used in future works forgross comparisons between different experimental methods and different subject groups, physiologicalor pathological.
As a first example, regarding physiological subjects, the average Vax of 0.60 mm/s measured by Waneket al. [32] and Jiang et al. [12] in diameters higher than 15 �m is approximately 27% lower than thatof 0.82 mm/s measured here in Group 3 (Fig. 2b). In addition, the average Vax of 0.32 mm/s measuredby Wanek et al. [32] in diameters of 11.2 (±0.9) �m is 50% lower than that of 0.64 mm/s measuredhere in Group 2 (Fig. 2b). Given that both Wanek et al. [32] and Jiang et al. [12] measured velocity withsemi-automated methods based on variations of the space-time image technique, these discrepancies maybe a result of the different measurement techniques.
As a second example, the average Vax value of 0.48 mm/s reported here for diameters between 4.4 and8.8 �m (Fig. 2b, Table 2), is more than double the average value of 0.19 mm/s reported by Ubbink et al.[29] at a diameter of 5 �m in the nail-fold of the big toe in the supine position. However, except fromthe fact that they measured at a different tissue, their measurements were from 16 asymptomatic patientswith a mean age of 70 years. In addition, some of them were under vasoactive medication and presentedsigns of atheromatic disease. Furthermore, they measured using the flying spot technique introduced byBasler (1919) which is a subjective technique accurate for very slow varying flows (periods longer than5 seconds).
Ubbink et al. [29] showed that video microscope velocimetry has predictive and discriminative powerto discern patients belonging to different Fontaine stages. However, a physiological reference of axialvelocity in relation to diameter from the human big toe nail-fold is missing.
Concerning pathological situations, Wanek et al. [32] found differences in the hemodynamic behaviorbetween SS and SC sickle cell disease patients, indicating a diagnostic potential of video microscopevelocimetry.
In conclusion, the results of this work showed the importance of measuring diameter and subdividingmicrovessels accordingly in hemodynamic studies either clinical or not. Higher diameters suggest higheraxial velocities but not for diameter changes less than approximately 5 �m in venules and 6 �m inarterioles.
References
[1] O. Arend, A. Harris, B.J. Martin and A. Remky, Scanning laser ophthalmoscopy-based evaluation of epipapillary velocities:Method and physiologic variability, Surv Ophthalmol 44(Suppl 1) (1999), S3–9.
[2] A. Basler, Uber die bestimmung der stromungsgeschwindgkeit in den blutkapillaren der menschlichen Haut, MunchnerMed Wschr 13 (1919), 347–348.
[3] A. Bollinger, P. Butti, J.-P. Barras, H. Trachsler and W. Siegenthaler, Red blood cell velocity in nailfold capillaries of manmeasured by a television microscopy technique, Microvasc Res 7 (1974), 61–72.

AU
THO
R C
OP
Y
A.G. Koutsiaris / Correlation of axial blood velocity to venular and arteriolar diameter 437
[4] P. Buti, M. Intaglietta, H. Reimann, C.H. Holliger, A. Bollinger and M. Anliker, Capillary red blood cell velocitymeasurements in human nailfold by videodensitometric method, Microvasc Res 10 (1975), 220–227.
[5] P. Charoenphol, R.B. Huang and O. Eniola-Adefeso, Potential role of size and hemodynamics in the efficacy of vascular-targeted spherical drug carriers, Biomaterials 31 (2010), 1392–1402.
[6] A.T.W. Cheung, P.C.Y. Chen, E.C. Larkin, P.L. Duong, S. Ramanujam, F. Tablin and T. Wun, Microvascular abnormalitiesin sickle cell disease: A computer assisted intravital microscopy study, Blood 99 (2002), 3999–4005.
[7] A.T.W. Cheung, M.M. Smith, P.C.Y. Chen, E. Miguelino, C.S. Li and S. Devaraj, Correlation of microvascular abnormalitiesand endothelial dysfunction in Type-1 Diabetes Mellitus (T1DM): A real-time intravital microscopy study, Clin HemorheolMicrocirc 42 (2009), 285–295.
[8] A.T.W. Cheung, B.S. Hu, S.A. Wong, J. Chow, M.S. Chan, W.J. To, J. Li, S. Ramanujam and P.C.Y. Chen, Microvascularabnormalities in the bulbar conjunctiva of contact lens users, Clin Hemorheol Microcirc 51 (2012), 77–86.
[9] A.T.W. Cheung, J.W. Miller, M.G. Miguelino, W.J. To, J. Li, X. Lin, P.C. Chen, S.L. Samarron, T. Wun, T. Zwerdlingand R. Green, Exchange transfusion therapy and its effects on real-time microcirculation in pediatric sickle sell anemiapatients: An intravital microscopy study, J Pediatr Hematol Oncol 34 (2012), 169–174.
[10] B. Fagrell, A. Fronek and M. Intaglietta, A microscope-television system for studying flow velocity in human skincapillaries, Am J Physiol 233 (1977), H318–H321.
[11] S. Forconi and T. Gori, Endothelium and hemorheology, Clin Hemorheol Microcirc 53 (2013), 3–10.[12] H. Jiang, J. Zhong, D.C. DeBuc, A. Tao, Z. Xu, B.L. Lam, C. Liu and J. Wang, A functional slit lamp biomicroscopy for
imaging bulbar conjunctival microvasculature in contact lens wearers, Microvasc Res 92 (2014), 62–71.[13] H. Jiang, Y. Ye, D.C. DeBuc, B.L. Lam, T. Rundek, A. Tao, Y. Shao and J. Wang, Human conjunctival microvasculature
assessed with a retinal function imager (RFI), Microvasc Res 85 (2013), 134–137.[14] H. Kang, H.I. Kwak, R. Kaunas and K.J. Bayless, Fluid shear stress and sphingosine 1-phosphate activate calpaine to
promote membrane type 1 matrix metalloproteinase (MT1-MMP) membrane translocation and endothelial invasion intothree-dimensional collagen matrices, J Biol Chem 286 (2011), 42017–42026.
[15] G.S. Kassab, Scaling laws of vascular trees: Of form and function, Am J Physiol Heart Circ Physiol 290 (2006),H894–H903.
[16] A.G. Koutsiaris and A. Pogiatzi, Velocity pulse measurements in the mesenteric arterioles of rabbits, Physiol Meas 25(2004), 15–25.
[17] A.G. Koutsiaris, Volume flow estimation in the precapillary mesenteric microvasculature in-vivo and the principle ofconstant pressure gradient, Biorheology 42 (2005), 479–491.
[18] A.G. Koutsiaris, S.V. Tachmitzi, N. Batis, M.G. Kotoula, C.H. Karabatsas, E. Tsironi and D.Z. Chatzoulis, Volume flowand wall shear stress quantification in the human conjunctival capillaries and post-capillary venules in-vivo, Biorheology44 (2007), 375–386.
[19] A.G. Koutsiaris, A velocity profile equation for blood flow in small arterioles and venules of small mammals in vivo andan evaluation based on literature data, Clin Hemorheol Microcirc 43 (2009), 321–334.
[20] A.G. Koutsiaris, S.V. Tachmitzi, P. Papavasileiou, N. Batis, M. Kotoula, A.D. Giannoukas and E. Tsironi, Blood velocitypulse quantification in the human conjunctival pre-capillary arterioles, Microvasc Res 80 (2010), 202–208.
[21] A.G. Koutsiaris, S.V. Tachmitzi and N. Batis, Wall shear stress quantification in the human conjunctival pre-capillaryarterioles in vivo, Microvasc Res 85 (2013), 34–39.
[22] A.G. Koutsiaris, The resistive index as a function of vessel diameter in the human carotid arterial tree, Microvasc Res 89(2013), 169–171.
[23] G. Landa, A.A. Jangi, P.M.T. Garcia and R.B. Rosen, Initial report of quantification of retinal blood flow velocity in normalhuman subjects using the Retinal Functional Imager (RFI), Int Ophthalmol 32 (2012), 211–215.
[24] L.C. Lo, K.C. Lin, Y.N. Hsu, T.P. Chen, J.Y. Chiang, Y.F. Chen and Y.T. Liu, Pseudo three–dimensional vision-basednail-fold morphological and hemodynamic analysis, Computers in Biology and Medicine 42 (2012), 873–884.
[25] P. Naik and L. Cucullo, In vitro blood-brain barrier models: Current and perspective technologies, J Pharm Sci 101 (2011),1337–1354.
[26] M. Shahidi, J. Wanek, B. Gaynes and T. Wu, Quantitative assessment of conjunctival microvascular circulation of thehuman eye, Microvasc Res 79 (2010), 109–113.
[27] M.M. Smith, P.C.Y. Chen, C.S. Li, S. Ramanujam and A.T.W. Cheung, Whole blood viscosity and microvascular abnor-malities in Alzheimer’s Disease, Clin Hemorheol Microcirc 41 (2009), 221–239.
[28] D.T. Ubbink, M.J.H.M. Jacobs, D.W. Slaaf, G.J.W.J.M. Tangelder and R.S. Reneman, Capillary recruitment and pain reliefon leg dependency in patients with severe lower limb ischemia, Circulation 85 (1992), 223–229.

AU
THO
R C
OP
Y
438 A.G. Koutsiaris / Correlation of axial blood velocity to venular and arteriolar diameter
[29] D.T. Ubbink, M.J.H.M. Jacobs, G.J. Tangelder, D.W. Slaaf and R.S. Reneman, The usefulness of capillary microscopy,transcutaneous oximetry and laser Doppler fluxmetry in the assessment of the severity of the lower limb ischaemia, Int JMicrocirc 14 (1994), 34–44.
[30] A. Uji, M. Hangai, S. Ooto, K. Takayama, N. Arakawa, H. Imamura, K. Nozato and N. Yoshimura, The source of movingparticles in parafoveal capillaries detected by adaptive optics scanning laser ophthalmoscopy, Invest Ophthalmol Vis Sci53 (2012), 171–178.
[31] F. Vozzi, F. Bianchi, A. Ahluwalia and C. Domenici, Hydrostatic pressure and shear stress affect endothelin-1 and nitricoxide release by endothelial cells in bioreactors, Biotechnology Journal 9 (2014), 146–154.
[32] J. Wanek, B. Gaynes, J.I. Lim, R. Molokie and M. Shahidi, Human bulbar conjunctival hemodynamics in haemoglobin SSand SC disease, Am J Hematol 88 (2013), 661–664.
[33] J.W. Warrick, E.W.K. Young, E.G. Schmuck, K.W. Saupe and D.J. Beebe, High-content adhesion assay to address limitedcell samples, Integrative Biology (Camb) 5 (2013), 720–727.
[34] C.C. Wu, G. Zhang, T.C. Huang and K.P. Lin, Red blood cell velocity measurements of complete capillary in finger nail-foldusing optical flow estimation, Microvasc Res 78 (2009), 319–324.
[35] Z. Zhong, B.L. Petrig, X. Qi and S.A. Burns, In vivo measurement of erythrocyte velocity and retinal blood flow usingadaptive optics scanning laser ophthalmoscopy, Opt Express 16 (2008), 12746–12756.